We are more often frightened than hurt;
and we suffer more from imagination than from reality.
Lucius Annaeus Seneca
How do you escape when intrusive thoughts and catastrophising invade?
I’m going to talk a bit about negative thoughts and how they affect you, and introduce you to Miranda K’s book Kill The Goblins: How to get the voices in your head to shut up, because I’ve suffered with my brain spiralling out of control since I was a child right through to late adulthood. Only recently have I found ways to combat the goblins, the brain weasels, the spectres, the ghouls, whatever you call them, in my head.
A study back in 2014 found that 94% of the UK population experienced unwanted and unpleasant thoughts: Did you lock your door when you left the house? What would it feel like to jump from a tall building? But these are passing thoughts that help us to recognise what is and what isn’t dangerous and our appropriate reactions to it. The thoughts in themselves are not the issue, they’re natural, it’s how you react to them that becomes the problem.
More serious negative thoughts can be a symptom of mental health conditions, most commonly Obsessive Compulsive Disorder (OCD) and Generalised Anxiety Disorder (GAD). People suffering with OCD and anxiety can question these thoughts, believing them or letting them lead to unhealthy urges or habits, which in turn steer them to more intrusive thoughts or catastrophising.
I was an introverted child with deep, imaginative, and invasive thoughts. At fourteen, I was repressed, had trauma, and had developed control-based disordered eating and self-harm. Intrusive thoughts were just part of me. I was that person who lay in bed, wide-eyed in the dark, unable to turn off my brain. Thoughts to self-harm, both physically and mentally, were already ingrained as was a great deal of fear. As an undiagnosed autistic I struggled with taking information at face value and being unable to read between the lines.
As a child and a teen I was a worrier, and then later I understood that most of my issues were with catastrophising. Fear of what could happen spiralling out of control in my mind.
This is just an example of one of my catastrophising episodes:
‘When my husband got a motorbike, years ago, there was always a risk he might have an accident, and most people would accept that and get on with their lives. Not me. When he left for the three mile journey to work at 6am, I would lay awake listening to his bike start up and move down the road. I could hear it turn the corner at the roundabout and then fade away. Instead of going back to sleep, I’d visualise his journey in my head. I’d see the next roundabout, then the next, then the stretch of bypass… and so on until he arrived at work ready to take his bus out.
But it wouldn’t end there. My brain would rewind and wonder if he’d actually made it to work. Somewhere along the route a lorry might have clipped the bike. My brain would show him mangled beneath it. Blue lights for an ambulance and blue lights for police at my door. Being told he was dead. I’d go through telling my kids, his family. I’d then go through the process of arranging a funeral, trying to work out what I’d live on. And by the time my brain had stopped with this charade I was a single parent, with no means to live and nothing to live for.’
Catastrophising, along with intrusive thoughts, is a poison.
Even as far as six or seven years ago I didn’t know much about catastrophising. My friend, Miranda, and I had often talked about mental health issues, and helped each other with what we knew. Miranda had a history of trauma, and a better understanding of negative thoughts and their consequences than I did. We talked a lot, and she helped me learn to understand catastrophising.
In 2019 I asked for referral for CBT to help with my excessive anxiety and catastrophising. I got referred to Integrated Psychological Therapies Services, who told me that everyone has and gets through negative thoughts. It didn’t matter how serious my thoughts were, that they also included self-harm and suicidal ideation, there was no help available.
I used a few of Miranda’s ideas and by the time I got a great counsellor, a year later, I’d learned to control a fair bit of my intrusive thoughts and catastrophising. My counsellor was impressed with how well I’d done in such a short amount of time. Along with medication, those tools changed my life.
I learned to recognise catastrophising and say ‘Stop!’, and then rewind what my brain was telling me, forcing it to play out in a normal way instead. So, with my husband and his motorbike journey to work, it would stop at arriving at work and his getting on with his day. The idea being that every time I began to catastrophise I would change the story so it would eventually become a non-story, and it would stop. This was my most effective tool and I’ve used it on all my negative and intrusive thoughts.
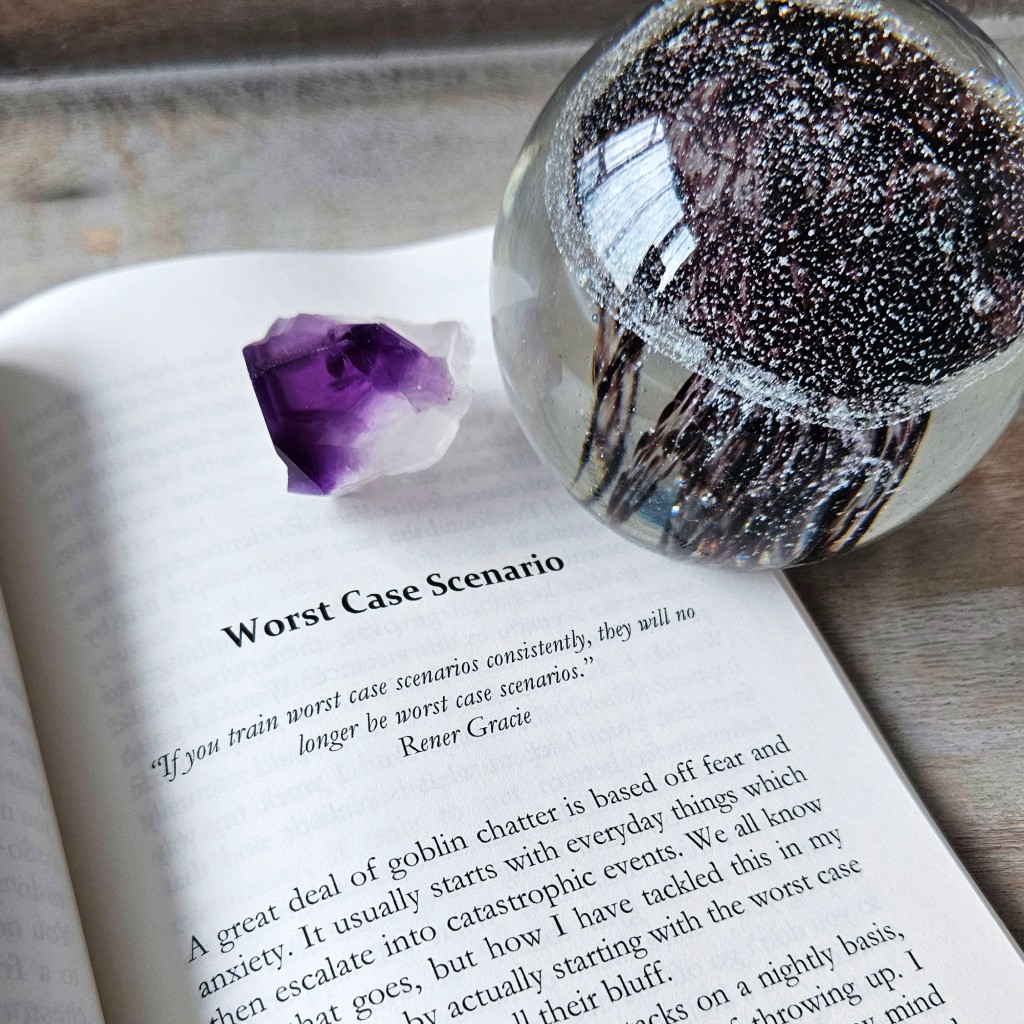
Miranda recently wrote a self-help book on this very subject: Kill The Goblins: How to get the voices in your head to shut up. It’s very accessible, written in a way to help you work out for yourself what will work best for your negative thoughts.
I decided to talk to Miranda and ask about how she chose to write this book:
I asked Miranda, who usually writes fiction with a good dose of horror or fantasy, what made her decide to write a self-help book, and why focus on negative thoughts?
There’s a lot to unpack there, so I’ll take it piece by piece. I’ve been an avid reader of self-help books most of my life, because I suffered a difficult and abusive childhood. I’m constantly working on healing the damage done to me and recovering myself. Writing fiction helps me escape from and also process some of the trauma, especially in my darker writing. It helps me put into words or in stories how it made me feel, and enables me to express feelings I wasn’t allowed to express as a child.
There is often a discussion about why people write horror or fantasy – or mix them together like me – and whether it relates to mental health. I actually wrote an article about this for a Horror review site called Ginger Nuts of Horror, and explained what led me to writing horror, and how it relates to my childhood, and why it is still my go-to genre as a reader. Find article here.
In terms of what made me decide to write my own self-help book, and why negative thoughts, the worst and most insidious part of the abuse I suffered was the verbal abuse which shows up later in life as negative self-talk in daily life – you basically replay all the awful things that were said to you, but in your own voice. Since I first went into therapy in my early twenties, initially due to daily panic attacks, I have been working to understand the patterns of behaviours and responses it has created for me, and retrain them. And during a breakdown in 2008 I was completely overrun with paranoid thoughts which led into suicidal ideation, although throughout I was conscious that it was how I was thinking, and I just needed to find someone who could help me change them. So I went into therapy and over six years of therapy developed the tools to do that and completely rebuild myself.
And now more than ten years on, I feel I’m on the other side of what I refer to as ‘the wall’, and realise I am not alone in having to be vigilant with my thoughts on a daily basis, several people around me also struggle, so after offering a few strategies I realised I had a lot of helpful knowledge, and decided this was what I needed to write about. And coupled with losing my mother in early 2021, I felt it was time I could finally share this with a wider more public audience.
Your book is called Kill The Goblins, how did you come up with the idea of using Goblins to personify negative thoughts?
Even though I make sure not to touch on any esoteric or ‘woo-woo’ in this book, I do dabble myself, and started using the term Goblins after reading a particular card in a set by Colette Baron-Reid called the Oracle Map. Card number 5 described them perfectly:
“Goblins are born when you’re wounded and something essential is lost in that experience. From that point on, as you forget your wholeness, they remain with you in the shadows. There they remind you of what brought them into being, by mimicking your own voice, tricking you into believing that you’re unworthy, victimised, or unlovable.”
I felt this encapsulated the mental image of the negative voices in my head, and how they left me feeling. And when others were coining phrases for the voices in their heads, this is the one I settled on. It also helps with the analogy throughout the book of how to go about killing them and stop feeding them.
That’s a briliant way to look at these kinds of thoughts. I’ve gone through major issues with catastrophising and intrusive thoughts myself, and when I read Kill The Goblins several of your coping methods were things I’ve actually used to combat my own mind’s negativity. You’ve utilised a great layout and accessibility to ideas and helps in the book – how did you decide what to include?
I brainstormed the ideas with a friend and wrote a list of all the strategies I had employed, and some of the more common ones. And as I was writing the book more appeared. I even found myself explaining to another friend how to prioritise and realised that was another one, and just kept adding to it until I had enough. I think it came out at around seventeen in the end.
I also touch on overused strategies, and some strategies that I hear people use but that aren’t necessary good in the long term, like demonising a part of yourself, and of course toxic positivity.
In terms of the layout, having read a lot of self-help books, I knew I wanted to cut out a lot of waffle and just get right down to the actual strategies, so the reader doesn’t have to try read between the lines to understand what to do. And a lot of people pick up and dip into self-help books, rather than read them cover to cover, so I wanted to make it accessible that way too.
Not everyone wants to get in depth about the whys and wherefores either, so I separated out the further discussion for later in the book. Chapter headings are very important to help the reader access the necessary information quickly too.
I know you’re very good with affirmations, how important is self-belief and positivity in your life?
I don’t know that I’m great at actively using affirmations, but what you think and say to yourself on a regular basis will affect your mood, your perspective and how you receive everything around you. We look through a lens that is tainted by our thoughts and feelings, so we always need to consider how we are tainting that lens – what we are saying to ourselves. So, finding words that support and help you on a daily basis, for me personally, are imperative.
I wouldn’t describe myself as a positive person per se, I’m a realist, often a sceptic, who will tend towards the negative, so I do have to work to keep an open and balanced mood and outlook. But over the last couple of years, I’ve found that when I do find myself giving a negative mental response to something external, I now have this other voice saying, but that’s not really fair, is it? And it offers a lighter, more positive outlook. I consider this to be a result of training myself out of the negative perspective point all the time, and consistently trying to look at myself and my life through a positive lens.
Self-belief has to be a constant for me. If I don’t believe in myself, no one else will – because there is literally no one else in my life supporting me emotionally. That has been a huge learning curve for me in recent years. And I have to believe in whatever it is I am working on, or I lose all interest and will end up resenting it. Supporting myself by being more ‘heart-centric’ has been a bit of a game changer. I now check in with how I feel about things, and ask myself if what I am doing is what I want to be doing. It also then changes my mood, because my outlook changes and I can be more positive.
So it’s sort of swings and roundabouts, but one feeds the other, like the snake eating its own tail.
What are your writing plans now? Will you extend your self-help work, or focus on fiction, or both?
I will be doing both! I am that meme with a load of noise spewing out the back of my head! My head is overrun with ideas, but for the self-help specifically I have two more books planned: one on anger and one on anxiety. I don’t have a timeline yet, but they will be produced in that order. They are both HUGE topics, and ones I have experienced, so I am sort of gestating on what strategies I use (if any) and how I can put it across in a book format to be helpful in the moment.
I also want to develop a course for people, but I am still honing in on exactly what the course would be about and how it will help people.
As for fiction: I’m writing the third book in a dark paranormal trilogy at the moment, I have a psych thriller waiting in the wings, an occult horror also vying for attention, and then I’ll be coming back round for another trilogy or series in the same world I am currently writing in! Phew! And who knows what might pop up in between! All part of a writer’s life.
Thank you, Miranda, I’m trying to keep a positive outlook too, working on keeping the negative thoughts quiet and offering myself a good supply of encouragment! It really helps.
I’ll add links at the end of this post for Miranda’s book and websites.
This book is a must-read for those who are struggling with negative and intrusive thoughts that spiral into a mess. It can also help those with anxiety and panic, as some of the ideas and tools can definitely be used to combat many other issues.
Several parts of her book have really helped me, including a section on reconnecting with what you’re feeling rather than what your thoughts are telling you, and having firm boundaries. I’ve been through religious trauma and sexual assault, and sometimes my fears and thoughts have been connected to those. Learning to allow myself to feel my emotions and listen to them, and how to eliminate guilt, has let me work out where some of my negative thoughts came from. This has allowed me to tackle them head on and to build a framework to work with.
I’ve also been able to understand that sometimes the thoughts aren’t just in my head, but society has chattering goblins all over the place, trying to shape us, condition us, and to climb into our heads! Being able to feel our own emotions, our own truths, and see the negativity and toxicity for what it is, and to set boundaries that are healthy is how we throw them back out and eradicate them. I realised I had the power to step away from some of my fear and hurt, and to shake it off.
Toxic positivity was also a chapter that revealed a lot to me. When people drain you with toxic positivity you doubt yourself, you lose self-worth, and your fears and negativity grow. Seriously, this book has helped me a great deal, even after counselling. I love my own personal power and the freedom it gives me to trust my own feelings, give them voice, and reconnect to them.
There are healthy ways to deal with negative contemplations, catastrophising, intrusive spirals, and trauma. If you can find a good counsellor, I recommend that, but as waiting lists are so long, Miranda’s book is a great place to start.
Have you had to deal with these issues? What helped you?
Links for Miranda K and Kill The Goblins: How to get the voices in your head to shut up –
Linktree for my fiction, Miranda Kate
Link to buy: Kill The Goblins: How to get the voices in your head to shut up – Available across all platforms and this is the best link to find them all.







































































 Meg’s mother is having a breakdown, and Meg can’t cope. Seeking to escape bullies and overwhelming anxiety, she discovers an old oak tree whose revelations begin to change her life.
Meg’s mother is having a breakdown, and Meg can’t cope. Seeking to escape bullies and overwhelming anxiety, she discovers an old oak tree whose revelations begin to change her life.







